Search
- Page Path
- HOME > Search
Original Article
- Bone Metabolism
- Comparison of the Effects of Various Antidiabetic Medication on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus
- Jeonghoon Ha, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Seung Hyun Ko, Moo Il Kang, Sung Dae Moon, Ki-Hyun Baek
- Endocrinol Metab. 2021;36(4):895-903. Published online August 9, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1026
- 6,168 View
- 230 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Prospective comparative studies on the effects of various antidiabetic agents on bone metabolism are limited. This study aimed to assess changes in bone mass and biochemical bone markers in postmenopausal patients with type 2 diabetes mellitus (T2DM).
Methods
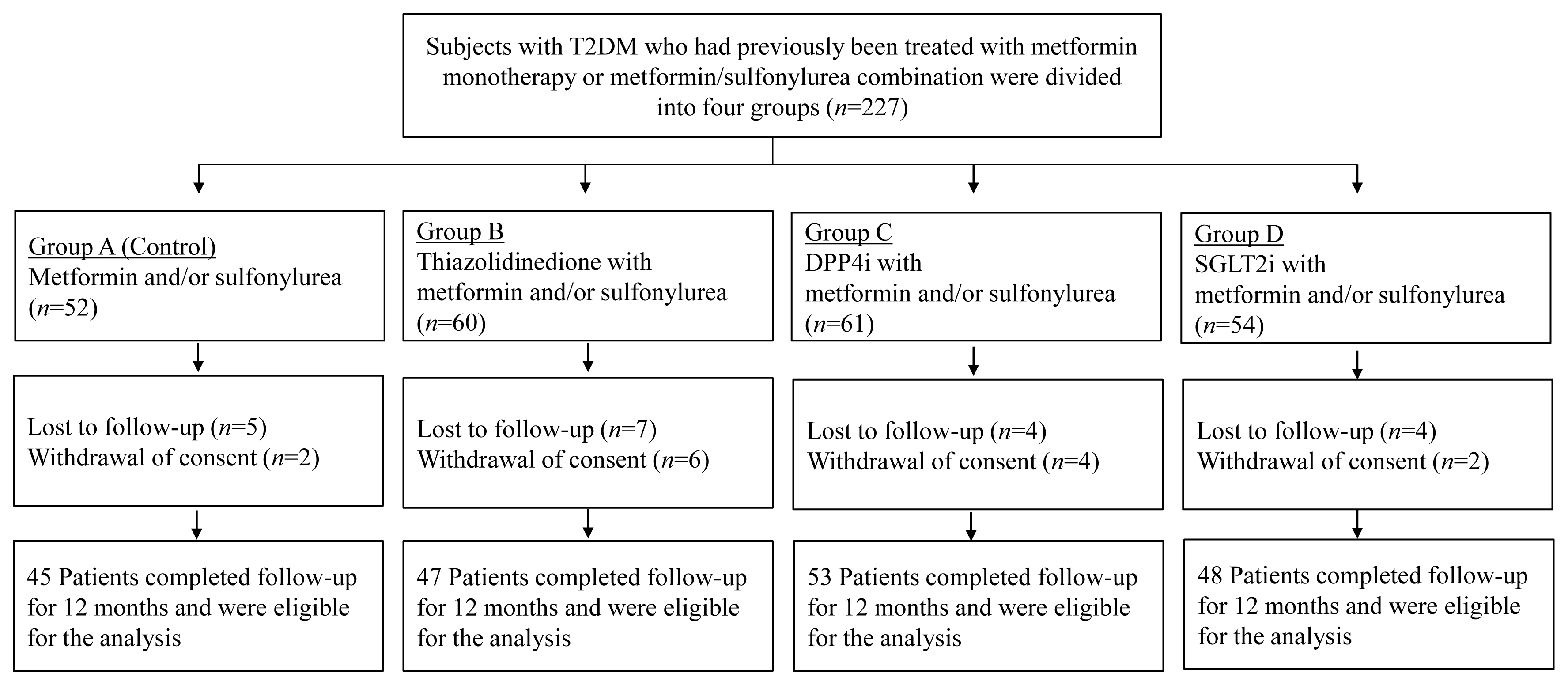
This prospective, multicenter, open-label, comparative trial included 264 patients with T2DM. Patients who had received a metformin, or sulfonylurea/metformin combination (Group 1); a thiazolidinedione combination (Group 2); a dipeptidyl peptidase-4 inhibitor (gemigliptin) combination (Group 3); or an sodium-glucose cotransporter 2 inhibitor (empagliflozin) combination (Group 4) were prospectively treated for 12 months; bone mineral density (BMD) and bone turnover marker (BTM) changes were evaluated.
Results
The femoral neck BMD percentage changes were −0.79%±2.86% (Group 1), −2.50%±3.08% (Group 2), −1.05%±2.74% (Group 3), and −1.24%±2.91% (Group 4) (P<0.05). The total hip BMD percentage changes were −0.57%±1.79% (Group 1), −1.74%±1.48% (Group 2), −0.75%±1.87% (Group 3), and −1.27%±1.72% (Group 4) (P<0.05). Mean serum BTM (C-terminal type 1 collagen telopeptide and procollagen type 1 amino-terminal propeptide) levels measured during the study period did not change over time or differ between groups.
Conclusion
Significant bone loss in the femoral neck and total hip was associated with thiazolidinedione combination regimens. However, bone loss was not significantly associated with combination regimens including gemigliptin or empagliflozin. Caution should be exercised during treatment with antidiabetic medications that adversely affect the bone in patients with diabetes at a high risk of bone loss. -
Citations
Citations to this article as recorded by- Meta-Analysis on the Association Between DPP-4 Inhibitors and Bone Mineral Density and Osteoporosis
Lili Huang, Wei Zhong, Xinghuan Liang, Huijuan Wang, Shi-en Fu, Zuojie Luo
Journal of Clinical Densitometry.2024; 27(1): 101455. CrossRef - A multicentre, double‐blind, placebo‐controlled, randomized, parallel comparison, phase 3 trial to evaluate the efficacy and safety of pioglitazone add‐on therapy in type 2 diabetic patients treated with metformin and dapagliflozin
Soo Lim, Seung‐Hwan Lee, Kyung‐Wan Min, Chang Beom Lee, Sang Yong Kim, Hye Jin Yoo, Nan Hee Kim, Jae Hyeon Kim, Seungjoon Oh, Jong Chul Won, Hyuk Sang Kwon, Mi Kyung Kim, Jung Hwan Park, In‐Kyung Jeong, Sungrae Kim
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Association of Bone Turnover Markers with Type 2 Diabetes Mellitus and Microvascular Complications: A Matched Case-Control Study
Yilin Hou, Xiaoyu Hou, Qian Nie, Qiuyang Xia, Rui Hu, Xiaoyue Yang, Guangyao Song, Luping Ren
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1177. CrossRef - Complementary effects of dapagliflozin and lobeglitazone on metabolism in a diet-induced obese mouse model
Yun Kyung Lee, Tae Jung Oh, Ji In Lee, Bo Yoon Choi, Hyen Chung Cho, Hak Chul Jang, Sung Hee Choi
European Journal of Pharmacology.2023; 957: 175946. CrossRef
- Meta-Analysis on the Association Between DPP-4 Inhibitors and Bone Mineral Density and Osteoporosis

Case Reports
- A Case of Sporadic Medullary Thyroid Cancer with RET G691S Polymorphism.
- Min Kyu Kang, Jung Min Lee, Ji Hyun Kim, Min Young Lee, Ji Hyun Kim, Sung Dae Moon, Je Ho Han, Sang Ah Chang
- J Korean Endocr Soc. 2009;24(4):293-297. Published online December 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.4.293
- 1,867 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Sporadic medullary thyroid carcinoma (MTC) is the most common form of MTC and somatic RET proto-oncogene mutations account for approximately 25% of the patients with sporadic MTC. However, other pathogeneses of sporadic MTC are still unclear. Not only RET mutation, but also polymorphisms of RET may have an association with sporadic MTC. We herein describe the association of MTC and RET proto-oncogene polymorphism. A 51-year-old man was diagnosed with MTC, which was incidentally found on a thyroid sonogram. The patient underwent total thyroidectomy and genetic mutational analysis of the RET gene. Genetic testing detected a polymorphism in codon 691 (G691S) on exon 11 of the RET proto-oncogene. His son and daughter had the same polymorphism. We report on this case along with a review of the related literature on RET gene polymorphism of sporadic MTC.

- A Case of Familial Multiple Endocrine Neoplasia with MEN1 Gene Mutation.
- Hye Young Sung, Yeon Joo Chun, Hyeug Lee, Bum Jun Kwon, Kun Woo Park, Jung Min Lee, Sung Dae Moon, Sang Ah Chang, Je Ho Han
- J Korean Endocr Soc. 2006;21(6):560-566. Published online December 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.6.560
- 1,830 View
- 27 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Multiple endocrine neoplasia type 1 (MEN 1) is an autosomal dominant disorder that's characterized by the combined occurrence of primary hyperparathyroidism, endocrine pancreatic tumors and anterior pituitary adenomas, but such manifestations as carcinoid tumors, adrenal adenoma and lipoma are also seen. We report here on a case of a 52-years old man with MEN type 1. He had a parathyroid adenoma, empty sella and a non-functioning pancreatic and adrenal mass. On the genetic analysis, he was proven to have a mutation in the MEN1 gene (exon 2, 200-201, INS AGCCC). On the family study for the mutation, one of his siblings and his son proved to have the same mutation.
-
Citations
Citations to this article as recorded by- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1
Yoon Jung Chung, Sena Hwang, Jong Ju Jeong, Sun Yong Song, Se Hoon Kim, Yumie Rhee
Endocrinology and Metabolism.2014; 29(3): 270. CrossRef - Endocrine Diseases in Diabetes Mellitus
Yongsoo Park
Hanyang Medical Reviews.2012; 32(4): 171. CrossRef - Somatic Mutational Analysis of MEN1 and Phenotypic Correlation in Sporadic Parathyroid Tumors
Young Su Chae, Hee Jin Kim, Sun Wook Kim, Myung-Chul Chang
Journal of the Korean Surgical Society.2009; 76(1): 15. CrossRef
- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1

- A Case of Atypical McCune-Albright Syndrome Associated with Hyperthyroidism.
- Yi Sun Jang, Seok Hui Kang, Woong Ryoung Jung, Woo Tae Kim, Hye Soo Kim, Jong Min Lee, Sung Dae Moon, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- J Korean Endocr Soc. 2006;21(2):158-164. Published online April 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.2.158
- 2,032 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - McCune-Albright syndrome (MAS) is a sporadic disease that's characterized by polyostotic fibrous dysplasia, cafe-au-lait pigmentation of the skin, and multiple endocrinopathies, including sexual precocity, hyperthyroidism, acromegaly, and hypercortisolism. Recent evidence has shown that the clinical manifestations are caused by a postzygotic activating missense mutation in the gene coding for the alpha-subunit of Gs protein that stimulates c-AMP formation in the affected tissues. Substitution of the Arg(201) residue in Gsalpha with cysteine or histidine have been identified in many MAS patients and Arg(201) to Gly or Leu mutations have also been recently identified. We identified the Arg(201) to His mutation in the gene encoding Gsalpha in the thyroid tissue from a 36-year-old man who was suffering with polyostotic fibrous dysplasia and hyperthyroidism.

Original Articles
- Korean Adult Growth Hormone Deficiency Treatment Registry.
- Sung Woon Kim, Seong Yeon Kim, Su Youn Nam, Yoon Sok Chung, Jae Hoon Chung, In Kyung Jung, Jong Ryeal Hahm, Minho Shong, Dong Sun Kim, Seong Keun Lee, Sung Dae Moon, Hyun Koo Yoon, Doo Man Kim, Sang Woo Kim, Hye Kyung Park
- J Korean Endocr Soc. 2002;17(1):43-47. Published online February 1, 2002
- 1,828 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Adult growth hormone (GH) deficiency is related with decreased lean body mass, increased body fat, and poor quality of life. In western countries, adult GH deficiency treatment registriesy provide a database of the effects and safety of GH deficiency treatment. The Korean Adult Growth Hormone Study Group of the Korean Society of Endocrinology register adult GH deficiency since 1996. METHEODS: Subjects were aged over 15 years, had organic hypothalamo-pituitary disease, and GH deficiency as documented by GH stimulation test or serum insulin-like growth factor-I (IGF-I) level. The underlying etiology for GH deficiency, serum IGF-I level, starting and maintenance dose, and adult GH deficiency assessment (AGHDA) score were investigated. RESULTS: From January 1996 to May 2001. 115 patients were enrolled. Mean age was 43.7 13.8 years and 60% were female. Thirteen medical institutions were involved in the registry. The most common underlying diseases were Sheehan's syndrome and pituitary adenomas. GH starting dose was from 0.4 to 1.0 units. Maintenance dose was between 0.5 and 1.2 units. Serum IGF-I levels were increased after GH treatment (0-week, 93.7 69.7 ng/mL; 2-weeks, 184.9 89.0 ng/mL; 6-weeks, 188.4 94.8 ng/mL; 10-weeks, 207.6 111.1 ng/mL; 6 months, 281.9 95.5 ng/mL). AGHDA scores slightly improved from 10.25 6.70 to 8.58 5.47 after 6 months of GH deficiency treatment. CONCLUSION: The GH Treatment Registry will be beneficial in monitoring the effects of GH deficiency treatment on Korean adult GH deficient subjects

- The Short-term Effects of Bone Marrow Transplantation on Bone Metabolism.
- Soon Jib Yoo, Yoo Bae Ahn, Kun Ho Yoon, Moo Il Kang, Kwang Woo Lee, Ho Young Son, Sung Koo Kang, Ki Ho Song, Yoon Hee Choi, Bong Yeon Cha, Hye Soo Kim, Ki Won Oh, Sung Dae Moon, Sang Ah Jang, Chun Choo Kim
- J Korean Endocr Soc. 1999;14(2):355-364. Published online January 1, 2001
- 1,128 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The organ transplantation becomes the management of choice for many patients with chronic and life threatening heart, liver, kidney, bone marrow, and pancreatic diseases. A new set of side effects unique to this groups of patients has become recognized. Bone disease is one of these complications. It is well known that there is an interplay between the cells in the bone marrow and the surrounding bone tissue. Marrow stromal cells include the progenitors of the osteoblastic lineage are the sources of effector molecules that support and regulate both hematopoiesis and bone remodeling. But little is known about the effects of myeloablative treatment followed by bone marrow transplantation(BMT) on bone metabolism. METHODS: We have investigated prospectively in 29 patients undergoing BMT(4 autologous, 25 allogenic) for hematologic diseases(19 leukemia, 9 severe aplastic anemia, 1 myelodyspoietic syndrome). Serum concentrations of calcium, phosphorus, creatinine, gonadotropins, sex hormones and biochemical markers of bone turnover(osteocalcin and carboxyterminal cross-linked telopeptide of type I collagen(ICTP)] were measured. The samples were collected before BMT and 1, 2, 3, 4, 12 weeks, 6 months and 1 year thereafter. Bone mineral density was measured with DEXA(Dual Energy X-ray Absorptiometry) before and after 1 year of BMT. RESULTS: 1. ICIP was progressively increased until 4 weeks after BMT when peak values were reached. And then decreased thereafter and basal values were regained after 1 year. Osteocalcin was progressively decreased until 3 weeks after BMT when nadir values were reached. And then increased thereafter and basal values were regained after 3 months. No distinct differences were observed in serum biochemical turnover marker between both sexes and between patients who received total body irradiation and those who did not. 2. Lumbar BMD was 2.1% decreased from 1.113 +/- 0.132 g/cm to 1.089 +/- 0.137 g/cm, and femoral BMD was 6.2% decreased fiom 1.078 +/- 0.156 g/cm to 1.011 +/- 0.157 g/cm. 3. 92% of the women (11/12) became menopausal manifested by high gonadotropin and low estradiol levels immediately after BMT. In contrast to women, gonadotropins and testosterone levels were not changed significantly in men after BMT. CONCLUSION: The rapid impairment of bone formation and also increase in bone resorption, as mirrored by the biochemical markers in this study, might play a role for the post-BMT bone loss. Further studies over many patients with a longer follow up will be needed.


 KES
KES

 First
First Prev
Prev



